Avoiding your Achilles' heel - Sports Medicine Doctor Malta - Dr Danica Bonello Spiteri
Main menu:
Avoiding your Achilles' heel
Avoiding your achilles heel (First published on vida magazine on September 2013)
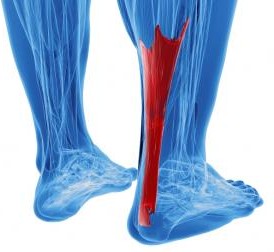
The Achilles tendon is located on the posterior aspect of the heel, as it descends down from the calf muscle in the lower leg. It is called the 'Achilles' after the legendary warrior, Achilles, in Homer's Iliad was shot in the heel with an arrow and died of the injury. Greek mythology states that his mother dipped him in a river when he was a child, to protect him from harm, but held him via the Achilles tendon, and this was his weak spot.
The Achilles is prone to injury as a result of repeated high loads, and athletes such as runners are very prone to this injury, although the general population is also prone to such injuries as a result of repeated use.
The commonest site of Achilles pain is in heel area, just above where the tendon attaches to bone, known as the mid-
The person suffering from this type of musculoskeletal problem experiences a gradual development of symptoms, intially with morning stiffness that eases off with movement, only to return once exercise is terminated. With the passage of time, the pain gets worse and eventually inhibits any type of pain free activity, as the tendinopathic process becomes more chronic in nature.
The previous misconception was that tendinopathies, such as this are due to an inflammatory process, so often anti-
There are various factors that cause Achilles tendinopathy, and no one single cause. Hence it is vital that each person is examined thoroughly in order to identify the cause and remove it.
Predisposing factors for this condition include, abnormal foot biomechanics (especially rolling the foot inwards, known as pronation), weak calf muscles, altered position of the lower leg bones (tibia and femur), genetic predisposition, male gender, being overweight, type II diabetes mellitus, prolonged years of running, poor muscle flexibility (tight calf muscles)and decreased movement in the ankle joint.
Additional changes to training regimes, such as a change in training ground surface, change in footwear, increased running mileage and decreased recovery time in between each training session are also risk factors in athletes.
Treatment of the condition will vary depending on the causative factor, as there are various options available. Strengthening exercises, mainly eccentric exercises (lengthening of the muscle), are essential.
Various injections have been proposed, with the aim of removing the painful nerves that are growing into the tendon itself.
Autologous platelet rich plasma, where a sample of blood is taken out from the injured patient, and then centrifuged so as to isolate the plasma. Plasma contains growth factors and this is then injected into the tendon in order to encourage regeneration and healing.
Extracorporeal shock wave therapy is aimed at increasing repair of the tendons as can also be utilised.
Treating the cause of the achilles tendinopathy may involve the expertise of a podiatrist, where the foot biomechanics and movements can be analysed in detail and corrected through use of insoles. This would aim to prevent a recurrence in the future.
Surgery as an option to treat Achilles tendinopathy has largely fallen out of fashion, as the outcome is no better than the above mentioned options, yet has greater risks and a much longer rehabilitation time to return to exercise.
However, the most crucial aspect of Achilles tendinopathy is to listen to that niggling sensation and get it treated in the initial stages, as if it becomes more chronic, it may prove harder and longer to rehabilitate.
For direct contact or to book a consultation please send an email on:
drdanica@sportsmedicinemalta.com
For direct contact or to book a consultation please send an email on:
drdanica@sportsmedicinemalta.com